‘Personalized’ education for patients with chronic pancreatitis
Author: Rupjyoti Talukdar
The mainstay of the management of chronic pancreatitis (CP) is medical therapy (analgesics, antioxidants, neuromodulators, pancreatic enzyme replacement), endotherapy (ERCP with or without pancreatic duct stenting, ESWL) and surgery (LPJ, Frey’s procedure, Whipple’s operation, distal pancreatectomy, total pancreatectomy). While each of these modalities have their benefits, none of these appears to be full proof for long-term amelioration of the most debilitating symptom, i.e. intractable pain. Several patients return with pain after any of these modalities, including total pancreatectomy (Figure 1).
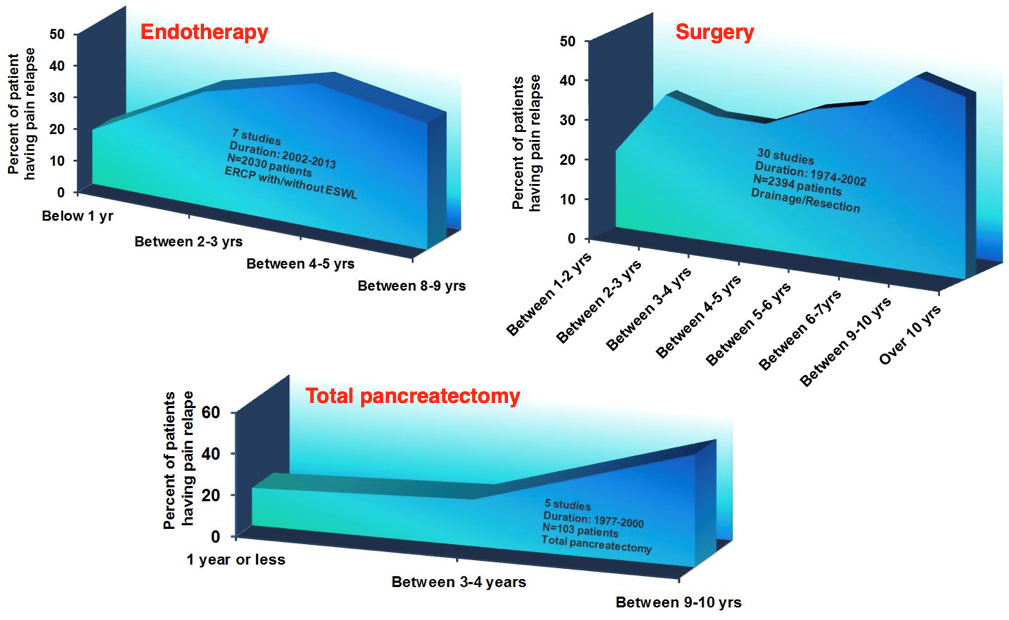
Figure 1: Recurrence of pain after pancreatic intervention in patients with chronic pancreatitis.
A deeper introspection will reveal that most of the above-mentioned modalities are directed towards the pancreatic morphological changes; and often the patient as an entity is overlooked. Chronic pancreatitis is a debilitatingly painful disease that lingers on for extended durations of time. The patient’s temporal perception of the disease could get shaped by diverse factors such as personality type, previous experience, educational level, inputs with peers, socio-cultural background, to name a few. This could explain why a few patients cope with the pain better, while others do not. Even though mechanisms of central neuropathy and neuroplasticity in chronic pancreatitis have been explained to a fair extent, much emphasis have not been laid on the areas of the brain responsible for pain modulation/processing, long-term pain memory and emotional responses to pain, i.e. the hippocampus.
Now there are data that clearly demonstrates alteration in metabolites in the hippocampus, basal ganglia, prefrontal cortex and the anterior cingulate cortex that correlates with depression, components of quality of life and pain scores in patients with chronic pancreatitis (Figure 2).
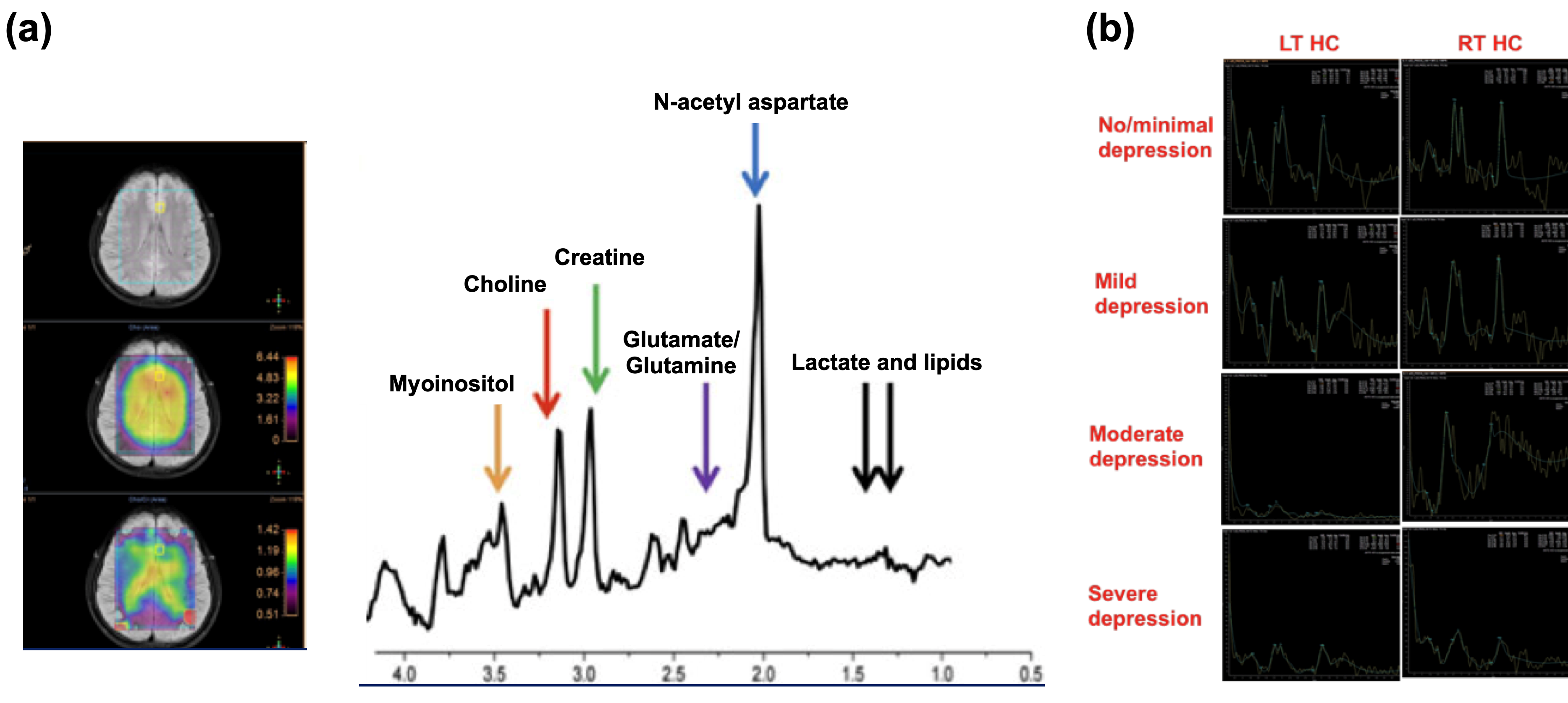
Figure 2: (a) Representative wave patterns of magnetic resonance spectroscopy (MRS) of the brain, (b) Magnetic resonance spectroscopic images of left and right hippocampus of patients with chronic pancreatitis with different grades of depression (as per Beck’s Depression Inventory score) and recurrent abdominal pain.
This leads to the question that could these changes contribute to the pain responses and thereby coping capabilities in these patients? With this background, when we counselled our patients and explained them their disease in an individualized manner based on their clinical manifestations and imaging correlates, we observed significant improvement in their depression scores, quality of life parameters and, most intriguingly, the pain scores. Repeat evaluation of the brain metabolites demonstrated substantial changes compared to baseline, and these correlated with the clinical parameters, including pain.
The aforementioned data reiterates the widely perceived (but diminutively practiced) importance of disease related education for patients with chronic pancreatitis. The data also provides mechanistic evidence with clinical correlates, which raise the hypothesis that appropriate or ‘personalized’ patient education, could not only comfort the patients or improve their perception about the disease, but also improve their pain coping capabilities thereby adding to the efficacy of the other modalities of treatment.
References:
1. S Sarkar, D Hazarika, A Atak, P Sarkar, M Khan, NR Duvvur, R Talukdar. Impact of Personalized Counseling on Depression and Quality of Life in Patients with Chronic Pancreatitis: Results from a Randomized Controlled Trial Gastroenterology, 2019; 156 (6): S-16 [Abstract].
2. S Sarkar, MR Goud, NR Duvvur, GV Rao, R Talukdar. Determinants of Depression and Its Impact on Quality of Life in Patients with Chronic Pancreatitis Gastroenterology 2018; 154 (6): S-202 [Abstract].